These 20 easy and delicious insulin resistance recipes for dinner are ready in up to 30 minutes and are diabetes-friendly. They are made with nutritious low to medium glycemic index foods.

Table of Contents
Watch us prepare one of our 20 insulin resistance recipes for dinner!
Best Foods For Insulin Resistance
Each of our insulin resistance diet recipes contains some of the best foods for insulin resistance:
- Leafy greens: Spinach, kale, and Swiss chard are nutrient-dense and have minimal impact on blood sugar.
- Whole grains: Quinoa, barley, and oats help stabilize blood sugar and avoid spikes. Thus, they are present in many of these high-fiber recipes and gut-healthy recipes!
- Legumes: Lentils, chickpeas, and black beans are high in fiber and protein, leading to better insulin levels.
- Nuts and seeds: Almonds, walnuts, chia seeds, and flaxseeds provide healthy fats and fiber. Keep in mind, nuts and seeds are high in calories and one should eat them in moderation.
- Lean proteins: Chicken, turkey, and fish are excellent protein sources as they don't contain high amounts of saturated fats, and also seafood which are rich in omega-3 fatty acids such as salmon and shrimp.
- Avocado: Avocados are high in monounsaturated fats, which can improve insulin sensitivity.
- Berries: Blueberries, raspberries, and strawberries all have a lower glycemic index compared to other fruits, making them a great option for salads and to add to your insulin resistance diet for weight loss. Try these anti-inflammatory recipes and this anti-inflammatory smoothie as a replacement for dinner!
- Vegetables: Balanced meals prepared with low to medium GI veggies such as broccoli, cauliflower, bell peppers, and eggplant are rich in essential nutrients yet lower on the glycemic index compared to veggies like potatoes.

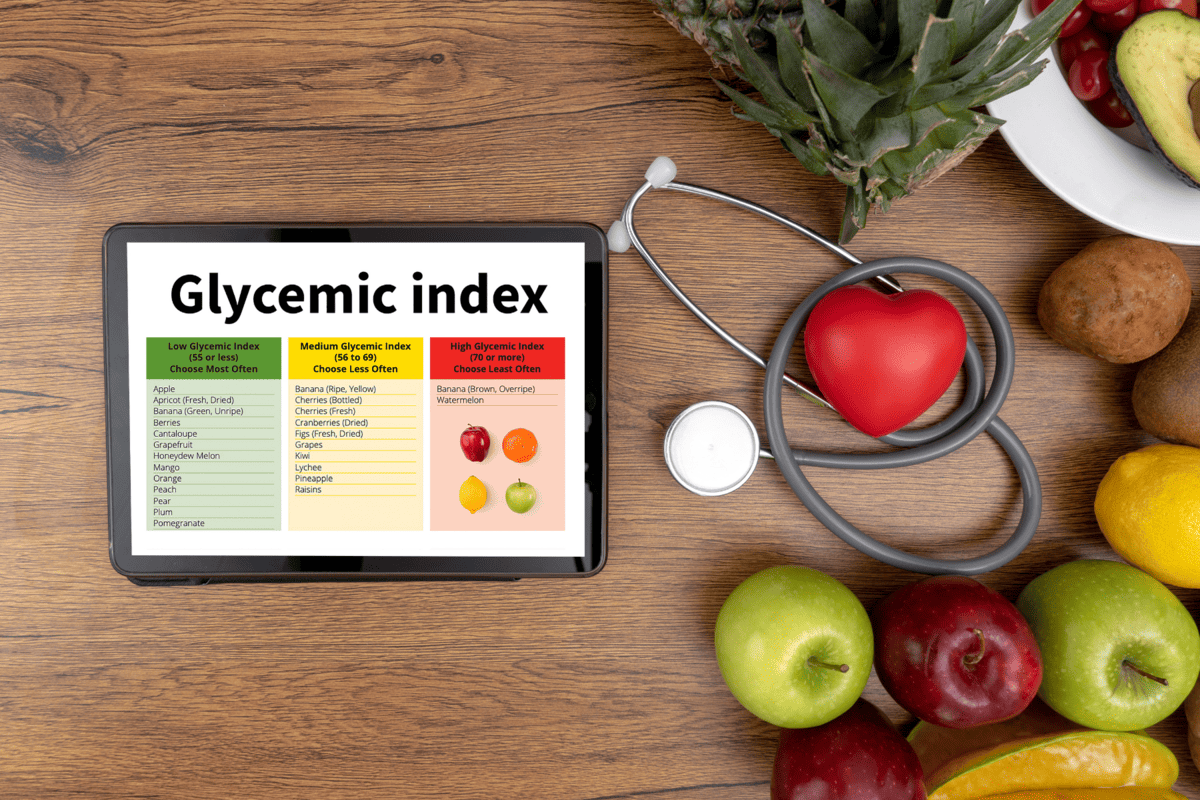
Understanding The Glycemic Index
The glycemic index (GI) is a scale that ranks a food containing carbohydrates by how much it raises blood sugar levels after it is eaten.
Foods with a high GI increase blood sugar higher and faster than foods with a low or medium glycemic index.
In other words, foods with a low glycemic index (0-55) and medium glycemic index (56-69) keep blood sugar more stable.
However, those with a high glycemic index (70 to 100) can be consumed in low to moderate amounts and in combination with lean protein or healthy fat. This helps slow down the digestion of carbs and prevent rapid spikes in glucose levels.
For more diabetes-friendly foods or ingredients to prepare other insulin resistance dinner meals, check out this glycemic index chart.
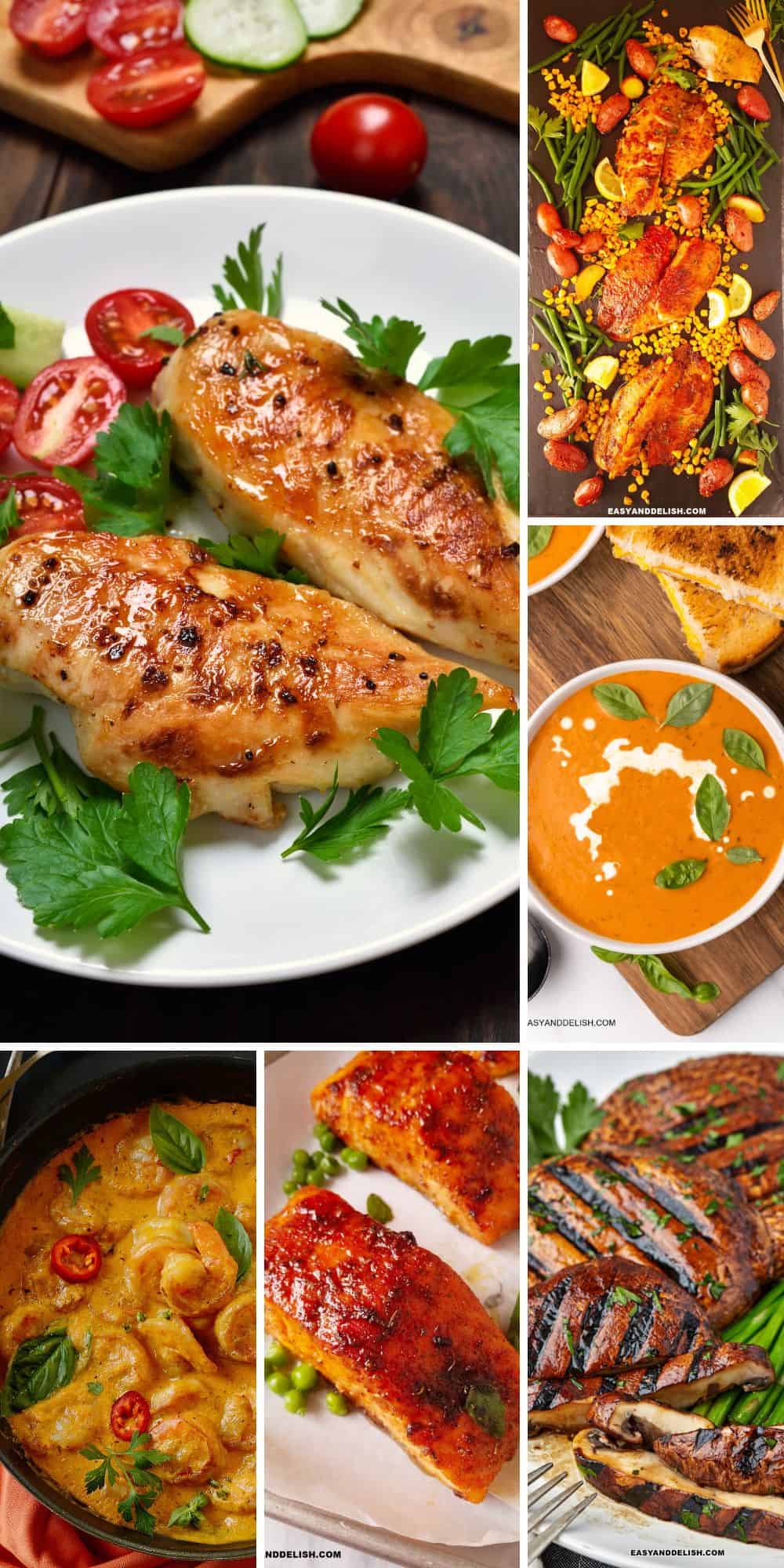
Insulin Resistance Diet Recipes
These quick and easy insulin resistance recipes are made with low to medium GI foods such as some whole grains, legumes, lean proteins, and healthy fats, making healthy dinner meals for busy weeknights. Therefore, add them to your meal plan or menu!

Chicken Fajitas
These lean protein-rich chicken fajitas call for skinless chicken breasts or thighs, spices, lime juice, and low-glycemic veggies such as onions and bell peppers. They are ready in 30 minutes and can be cooked on the stovetop or baked in the oven. Serve them with whole wheat tortillas, pico de Gallo, sour cream, and guacamole, or with refried or black beans and this cauliflower cilantro lime rice.
Pizza Toasts
Our 20-minute pizza toasts have toasted sourdough bread topped with pizza sauce and a Mediterranean salsa. Thus, it is a quick and simple insulin resistance recipe for busy weeknights.
Weight Loss Cabbage Soup
Loaded with non-starchy vegetables, this low-carb vegetarian cabbage soup makes a 30-minute budget-friendly dinner for meatless Mondays. It is also anti-inflammatory, detox, and rich in antioxidants!
Baked Blackened Salmon
Our baked salmon recipe is rich in omega-3 fatty acids and calls for a blend of homemade blackened seasonings, making a delicious 20-minute dinner that is perfect for a large family or a weekly or monthly meal prep. Pair it with this healthy side of air fryer asparagus for a complete meal.
Cajun Shrimp Pasta Recipe
It has shrimp seasoned with Cajun seasonings, sauteed for 3-4 minutes, and then tossed with whole wheat pasta in a creamy sauce. This healthy pasta dinner takes about 25 minutes to be ready!
Shrimp and Asparagus
This sheet-pan shrimp and asparagus is ready in 25 minutes and is prepared with lemon juice, garlic, Parmesan cheese, olive oil, and seasonings. It makes a hassle-free, healthy dinner for busy days. For a more fulfilling meal, you may pair it with this side of pearl barley recipe (26 g net carbs/163 calories) that you can prep ahead though.
Norwegian Fish Soup Recipe
Our 25-minute fish soup calls for salmon, non-starchy vegetables (onion, garlic, cauliflower, and leeks), spices, herbs, and cream which you can replace with Greek yogurt though. It makes a healthy comforting dinner for insulin resistance!
Baked Chicken Breast Recipe
Do you enjoy meal prepping for the week? This 30-minute skinless baked chicken breast made with 3 ingredients is a main dish that pairs well with any non-starchy vegetable, a whole grain side such as brown rice, or this cannellini bean salad. Other diabetes-friendly serving suggestions are mashed cauliflower, Thomas Keller zucchini, zoodles, in rye bread sandwiches, or more.
Air Fryer Tilapia Recipe
Tilapia filets seasoned with Cajun seasonings and cooked in the air fryer for an easy dinner meal that is ready in 20 minutes. Pair this lean protein main dish with steamed green beans or a green salad, and enjoy a light meal packed with flavor. Or if you prefer a more substantial meal, serve it with this grilled corn on the cob which has a 52 GI (low-glycemic) according to Healthline.
Instant Pot Tomato Soup Recipe
This tomato soup is a twist on a classic that never gets old! Our 30-minute dinner meal is pure comfort and flavor. Pair it with sourdough toast or a grilled cheese made with 100% whole wheat bread.
Shrimp in Coconut Sauce
This 30-minute tropical dinner has shrimp cooked in a creamy sauce made with blended non-starchy veggies and coconut milk. It is a restaurant-quality meal best served over brown rice or whole wheat pasta and so perfect for those with insulin resistance.
Air Fryer Salmon Recipe
Love salmon? How about crispy Cajun salmon filets cooked in the air fryer? It is a flavorful 15-minute insulin resistance recipe for dinner that everyone loves and can be served with quinoa, air fryer zucchini fries, or air fryer broccolini.
Mushroom Steak Recipe
Ready in just 30 minutes, this grilled mushroom steak makes a flavorful Asian vegan dinner for summer or any time of the year. You can have it with zoodles, as a sandwich filling between 2 slices of this sourdough bread, or this Instant Pot Brussels sprouts.

Cauliflower Steak Recipe
Baked or grilled, this 30-minute cauliflower steak is a meatless dinner that will help you achieve your health goals. Serve it with chimichurri sauce and steamed asparagus or green beans, or this cucumber chickpea salad.
Instant Pot Lentils
This flavorful Moroccan stew with brown lentils, sweet potatoes, celery, onion, tomatoes, and a blend of spices is rich in plant-based protein and fiber, making it one of those easy insulin resistance recipes that are ready in 25 minutes. Serve it over basmati rice and whole wheat naan or pita.
Butter Bean Curry
A comforting vegan dinner meal for busy evenings, this soulful butter bean curry with non-starchy veggies, spices, coconut milk, and vegetable broth is ready in just 20 minutes. But for a complete meal, serve it with brown rice and whole wheat naan.
Beef and Broccoli Stir Fry
This 30-minute meal comes packed with lean beef, broccoli, and a delicious homemade Asian sauce, making the perfect insulin resistance dinner recipe for blood sugar control!
Italian Baccala
Our 30-minute baked cod in wine sauce with capers, tomatoes, and basil makes a summery dinner meal with fresh flavors. Thus, it pairs well with quinoa, toasted sourdough bread, or whole-wheat pasta.
Shrimp Scampi Pasta
Our one-pot Italian dinner has whole-wheat pasta tossed in a creamy sauce, making a comforting meal that is ready in just 20 minutes. Pair this one-dish meal with a green salad or whole wheat baguette.
Mushroom Curry
Make this budget-friendly vegan curry with mushrooms, broth, coconut milk, spices, and curry powder on the stovetop or Instant Pot in 15 minutes. I enjoy serving it over basmati rice or with a side of whole wheat naan.
Other Healthy Recipes for Dinner
- 75 Easy dinner ideas
- 80 Low-calorie dinner recipes
- 30 Low-carb dinners
- 25 Easy healthy dinners for two
- 50 Easy gluten-free dinner recipes
- 30 High-protein dinners
- 30 No-cook meals
- 70 Easy chicken recipes for dinner
- 55 Easy beef recipes for dinner
PIN AND ENJOY!
20 Insulin Resistance Recipes for Dinner
Equipment
- 1 pressure cooker
Ingredients
- 1 teaspoon olive oil
- 1 medium onion diced
- 1 lb mushrooms sliced
- 2 garlic cloves minced
- 1 tablespoon grated fresh ginger
- 2 tablespoon curry powder
- ¼ teaspoon chili powder
- 1 ½ cups tomato sauce
- 2 tablespoon tomato puree or paste
- ¾ cup full-fat coconut milk
- ¼ cup vegetable stock or broth
- 1 lime juiced
- 2 tablespoon chopped cilantro
Instructions
- Press the sauté function and let it heat for about 5 minutes. Pour the oil and cook the onion for about 3 minutes, stirring often to keep from browning. Add the mushroom and cook for about 2-3 minutes, stirring every now and then. Add the garlic and ginger and cook for 1 minute.
- Then stir in both the curry powder and chili powder, the tomato sauce and puree, coconut milk, and stock.
- Cancel the sauté function, lock the lid, turn the valve, and set on manual high pressure for 3 minutes. If you have a pressure cooker, you may press the stew button and then manually set for 3 minutes. Do a quick release.
- Then stir in the lime juice and serve with the cilantro on top.
Recipe Video
Recipe Notes
- Heat a nonstick pot or Dutch pan over medium heat, add the oil and cook the onion for about 3 minutes, stirring often to keep from browning. Add the mushroom and cook for about 2-3 minutes, stirring every now and then. Add the garlic and ginger and cook for 1 minute.
- Then stir in both the curry powder and chili powder, the tomato sauce and purée, coconut milk, and stock.
- Increase the heat to medium-high and bring to a boil. Then reduce the heat to medium-low, cover, and let it simmer for about 10 minutes. Stir in lime juice and serve with the cilantro on top.
- Store mushroom curry in an airtight container in the fridge for up to 4 days.
- You may freeze it for up to 2 months but be aware that once thawed it becomes a bit watery. One thing that you can do to fix it, it is to reheat, uncovered, over low heat, and let the sauce reduce a little bit. Then stir well a few spoonfuls of either coconut cream or yogurt. They have a thick consistency and will make the curry creamy again.
Nutrition
** Nutrition labels on easyanddelish.com are for educational purposes only. This info is provided as a courtesy and is only an estimate, since the nutrition content of recipes can vary based on ingredient brand or source, portion sizes, recipe changes/variations, and other factors. We suggest making your own calculations using your preferred calculator, based on which ingredients you use, or consulting with a registered dietitian to determine nutritional values more precisely.
Please note that health-focused and diet information provided on easyanddelish.com is for educational purposes and does not constitute medical advice, nor is it intended to diagnose, treat, cure, or prevent disease. Consult with your doctor or other qualified health professional prior to initiating any significant change in your diet or exercise regimen, or for any other issue necessitating medical advice.
This post was first published on August 14, 2023.







Kechi says
This is such an informative post, and amazing nutritious recipes! I look forward to trying the butter bean curry this weekend! Also, thanks for including my recipe, Denise!
Denise Browning says
Thank you Kechi! I am happy you find our insulin resistance recipes useful. I also appreciate your feedback and contribution!